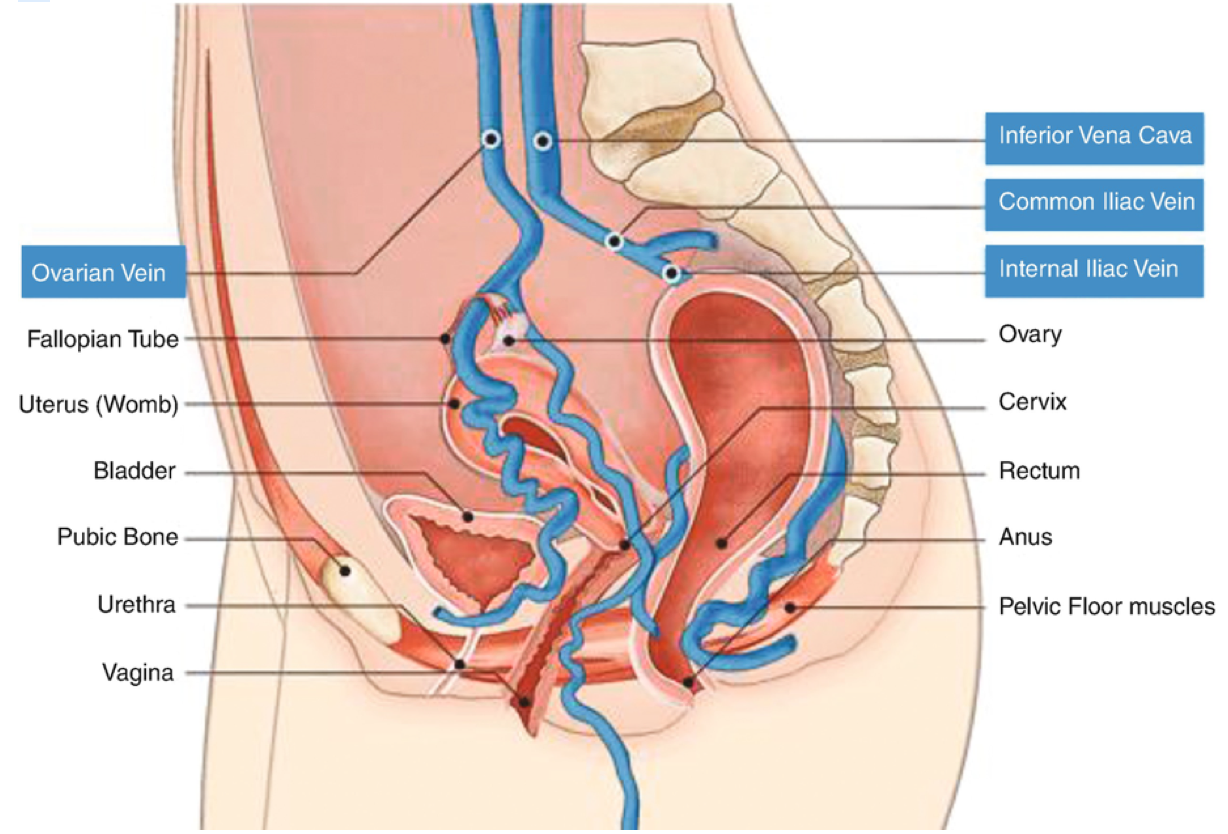
Vulval varices, sometimes referred to as vaginal varicose veins are found on the labia majora and minora. Vulval varices are dilated venous channels that most likely develop from combination of both, proximal vein obstruction and damaged valves, which cause increased pressure in venous system.They usually occur during pregnancy and typically regress spontaneously within six weeks after giving birth. When they occur in nonpregnant women, they generally present in the second or third decade of life. It is estimated that 4% of women have had vulval varices. They may be isolated or associated with varices of the leg , and they may occur as part of Pelvic Congestion Syndrome.
What are vaginal and vulval veins?
Why are vulval veins more common in pregnancy?
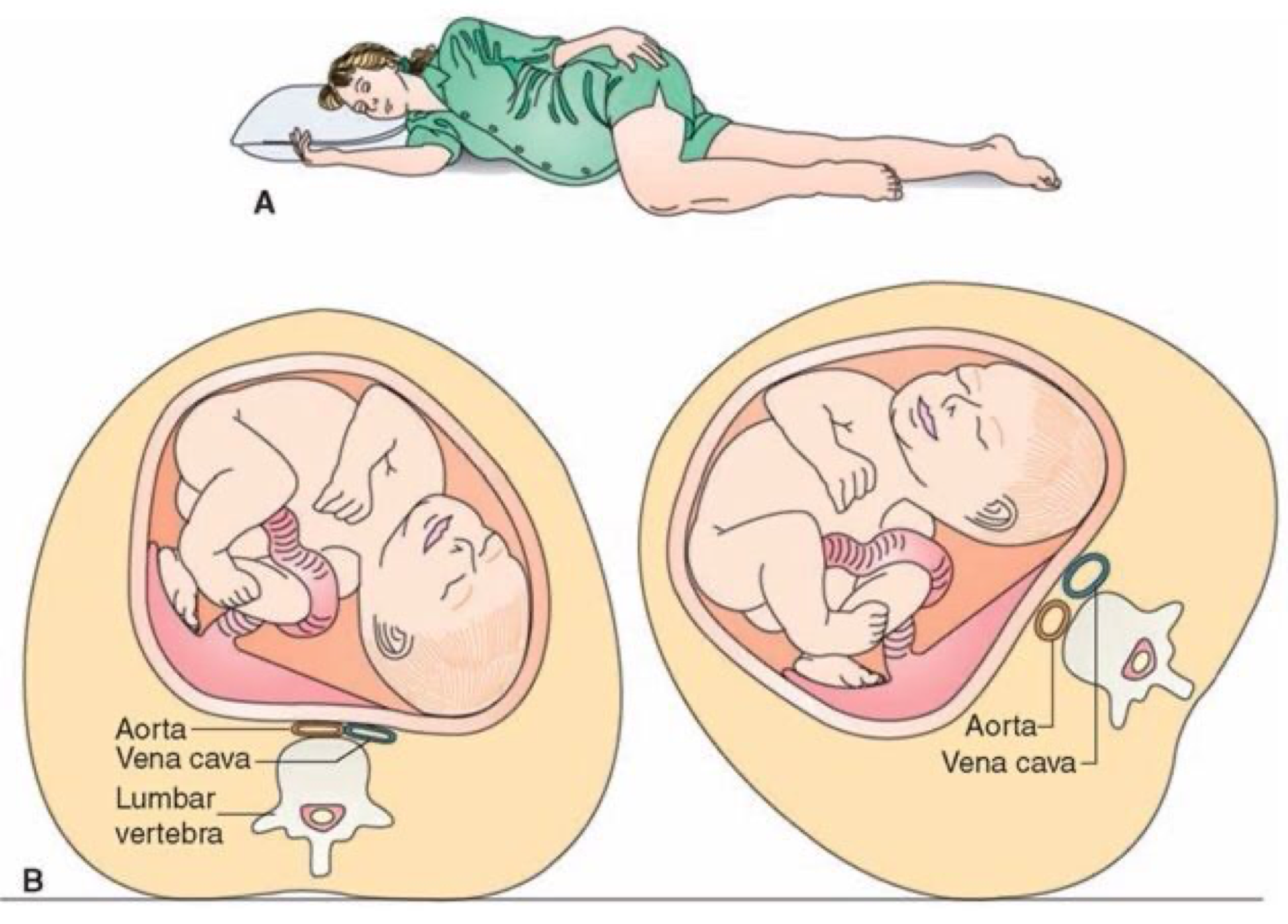
Vulval veins are most common in pregnant women ad they occur typically within the last trimester, affecting approximately 18-22% of population. Vulval varices are usually caused by leaking valves within the pelvic area, rather than on the legs. This is due to the increased blood flow in pelvis which is associated with the decrease venous return from the lower body to the heart as a result of mechanical compression of large veins such as vena cava and iliac veins from the baby and the expanding uterus. Increased venous pressure results in blood pools in the veins of your legs as well as your vulval region, causing varicosities. Additionally changes in hormone balance can trigger these veins to dilate and store more blood, leading to a weakening of the walls and enlargement of the vessels in the vulva. Pelvic vein reflux is common during and after pregnancy, especially in women who have delivered a natural birth. It can be one of the triggering factors to get varicose veins in legs and vulva. When this happens, it’s particularly difficult to treat the veins. Moreover, these tend to reoccur more often within the top of the thigh. Vulval varices are often very sore and may bleed during the delivery of the baby.
Vulvar varicosities are not usually permanent. Symptoms typically disappear shortly after giving birth. However, women who get them during one pregnancy may develop them with the next pregnancy. The veins and symptoms may get worse or more painful with every additional pregnancy becoming more significant.
What are the signs and symptoms of vulval varicosities?
Vulval varicosities don’t always cause signs and symptoms. You can have vulval varices and not be aware of them, as they are not always visible. In severe cases, the dilated vessels can bulge and look bluish and feel bumpy. If they occur, they might include a feeling of:
- Pain and/or swelling in vagina or vulva
- Pain that gets worse after standing, sexual intercourse or exercise
- The sensation of pressure or fullness in the genitals
- Urinary urgency or pain
- Hemorrhoids ad/or rectal pain
- Visible tortuous and bulging veins in the genitals and/or atypical locations of leg along with swelling
More severe cases include bulging visible veins on or near the genital area. In pregnancy varicose veins in the legs are very common. Some research studies show that up to 20% of women with varicose veins in the legs, also, have vulvar and pelvic veins. For some women, these veins subside on their own after giving birth. If not, it could be in indication of Pelvic Congestion Syndrome.
Pelvic Congestion Disorder symptoms include:
- Pelvic pain similar to contractions or a heavy menstruation
- Painful intercourse
- Pain in the pelvic area and legs after intimacy
- Abdominal bloating ad constipation
- Difficult or painful urination
What diagnostic tests are used for vulval varicose veins
The first way to diagnose this medical condition is by simply looking. In some women the varicose veins are restricted to the vulva area whereas in others they lead to varicose veins formation in the inner part of the thigh next to the vulva or to veins down the back of the thigh. To establish diagnosis, the communication from the atypical varicose veins in the legs to the ovarian veins or pelvic veins reflux must be shown and incompetence of one or both ovarian veins must be demonstrated. When vulval varicose veins have been seen or when atypical varicose veins appear in the legs, and ovarian or pelvic vein reflux is suspected, a specialised ultrasound examination, called Trans-vaginal Duplex Ultrasound (TVS) is required using a special probe that can see veins through vagina.
Other imaging tests may be needed to confirm the final diagnosis. These studies may include venography with intention to treat, computed tomography (CT) or magnetic resonance imaging venography (MRI) for visualization of dilated veins and surrounding anatomical structures.
Clinical grading scale for varicose veins of the vulva
Vulval varicosities varies and severity is graded on a scale of one to four. Those with the milde form (Grade 1) are usually unaware that they are present and the diagnosis is usually made by ultrasound when investigating for leg varicose veins. Once they become visible, they are graded upwards from two to four. Prevalence
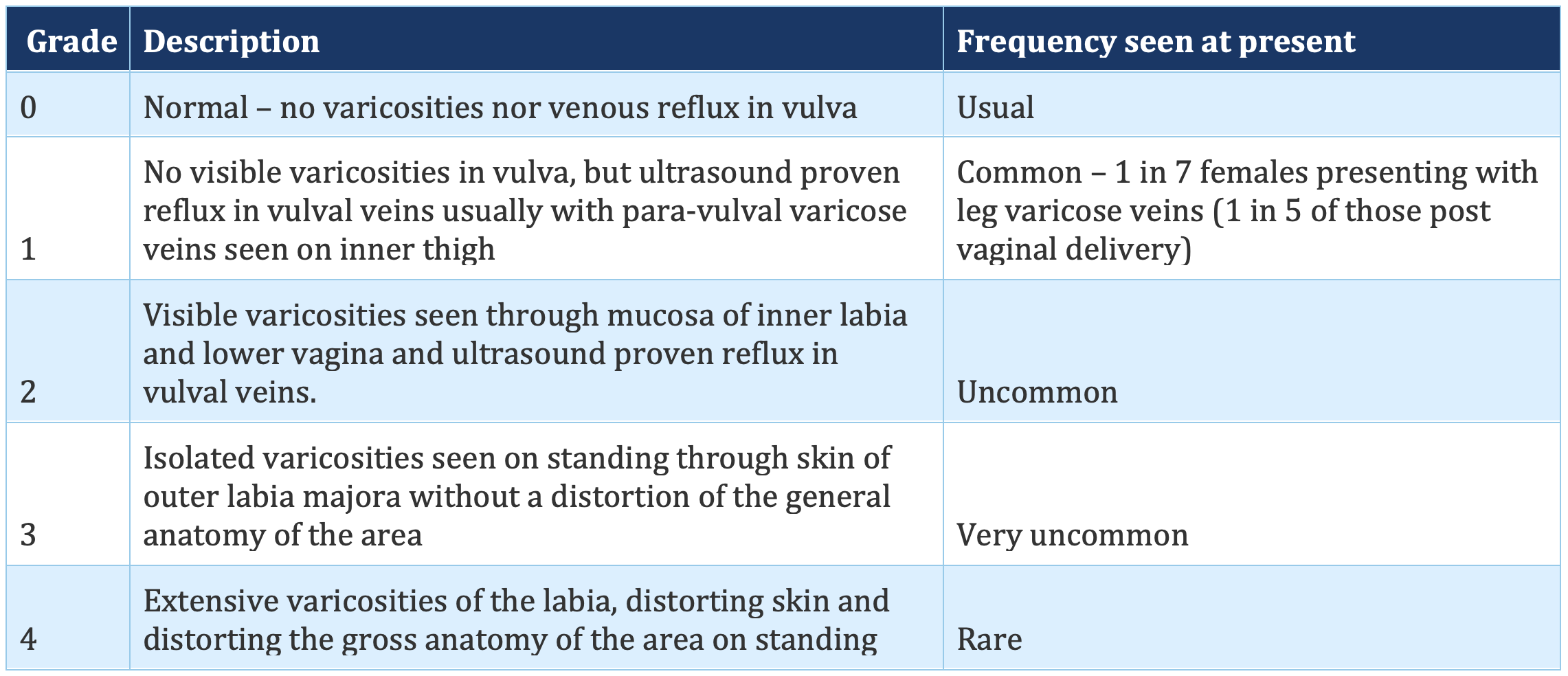
is uncommon and fewer women are likely to have the higher grades.
The below is widely recognized grading scale for vagina and vulval varicose veins published for medical and therapeutic purpose, and used to classify the severity of any patients presenting with varicose veins of vulva.
Which treatment is best for you?
Most doctors or surgeons who treat varicose veins either do not know that there is an effective treatment for this condition or treat them by removing these veins from vulva and/or the top of the thigh, or even injecting them before properly diagnosing the underlying cause of this problem. Often, these patients present to the vein clinic with recurrent varicose veins, because the standard procedures have failed and the pelvic origin was not recognised. Thus the understanding of the venous pathology plays essential role in successful treatment .
By using our experience, knowledge and well recognized techniques with multispecialty team approach we are capable of identifying the exact cause and then treat it effectively, using the latest non-invasive diagnostic techniques and minimally invasive treatments.
The initial treatment for vulvar varicosities with pelvic symptoms may include preventive measures to bring relief and reduce pain.
- Leg elevation to promote better circulation and changing your position more often to prevent blood pooling
- Wearsupport garments designed to reduce groin and leg vein pressure
- Apply cold compresses to your vulva. This might ease your discomfort.
- Healthy weight management
- If you’re pregnant, wear a support underwear and also sleep on your left side to promote better blood circulation (this places less pressure on vena cava)
- Avoid sitting or standing for long periods of time
- Drink plenty of fluids
When the veins do not disappear on their own, it is important to consult your doctor about possible underlying causes and best treatment. Vascular surgeon can easily remove the veins with minimal invasive procedures however, do not recommend removing vulvar varicosities during pregnancy since they may go away on their own. If the veins do not disappear a few weeks after giving birth, surgical procedures can be used for definitive treatment.
If you have vulvar varicosities along with leg varicose veins, your symptoms help determine the best treatment approach. With limited pelvic venous reflux, the leg veins are often treated first.
If your vulval varicose veins and pelvic symptoms are more severe, procedures treating the pelvic veins may be recommended before treating your legs veins.
The treatment of choice involve initially performing a diagnostic venogram with contrast to identify the cause of the pelvic veins followed by minimally invasive endovascular procedures to correct the unhealthy pelvic veins in form of coil embolization and/or sclerotherapy. Having removed the cause and relieved the pelvic symptoms, the leg veins can then be successfully treated.
These two most commonly performed procedures use either a catheter to close damaged veins with a coil and or involves injection of a foam solution into the vein that blocks blood flow, eliminating the pain and swelling.
Both procedures are safe and effective, usually performed under local anesthesia via groin access and may require overnight stay at the hospital.

